As part of this effort, we retired certain fax numbers for medical prior authorization requests in 2019, and asked you to use the prior authorization and notification tool on link — the same website you use to check eligibility and benefits, manage claims and update your demographic information.
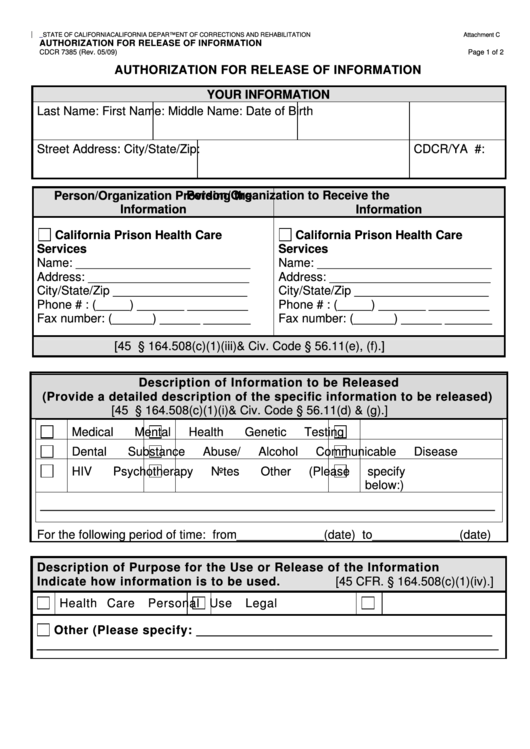
Notwithstanding any provision of this chapter and section 351 of the public health service act [42 u. s. c. 262], and subject to the provisions of this section, the secretary may authorize the introduction into interstate commerce, during the effective period of a declaration under subsection (b), of a drug, device, or biological product intended for use in an actual or potential emergency. 56. 10. (a) a provider of health care, health care service plan, or contractor shall not disclose medical information regarding a patient of the provider of health care or an enrollee or subscriber of a health care service plan without first obtaining an authorization, except as provided in subdivision (b) or (c). The authorization code ranges will assist in administering benefits. information on this site is for informational purposes only and does not guarantee coverage or payment. all benefits are subject to the patient’s medical coverage agreement including visit, quantity, and/or dollar limits.
Authorizations Providers Excellus Bluecross Blueshield
Medical Provider U S Department Of Labor


Medical Policy Outpatient Prior Authorization Code List
Click on the title for complete list of drugs that require prior authorization: medical benefit prior authorization medication list, 034 medical utilization management and pharmacy prior authorization, 033 policy number and title products procedure codes 008 zolgensma (onasemnogene abeparvovec-xioi) for spinal muscular atrophy. Medical technology assessment non-covered services list, 400 the table below represents medical policies with corresponding specific procedure codes. these procedure codes require prior authorization when they are performed in the outpatient setting. if the procedure codes that are listed in this document are performed in the inpatient setting,.
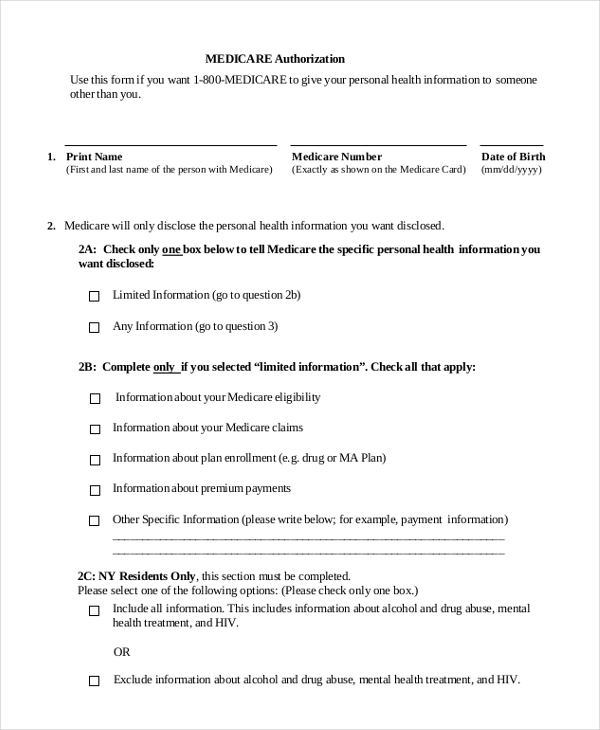
So authorization is must to treat certain services to patient in order for provider to get reimburse the claim. there are 2 types of authorization in medical billing: prior authorization; retro authorization; prior authorization: prior authorization also called as pre authorization. physician has to obtain permission for certain health care. Medical authorizations & claimsauthorization process. all requests for ccs diagnostic and treatment services must be submitted using a service authorization request (sar) form except orthodontic and dental services (all necessary authorizations will be medi-cal dental ’s responsibility). only active medi-cal providers may receive authorization to provide ccs program services. Nov 14, 2018 · (2) the responsibility for organization and conduct of the medical staff shall be developed and defined in writing in consultation with the medical staff and assigned to the medical director who is a physician appointed by the governing body in accordance with section 405. 2(e)(2) of this part, based upon written qualifications for the position.
Medical health procedure codes requiring prior authorization: medical prior authorization code list may 1, 2021 open a pdf medical prior authorization code listfebruary 23, 2021 open a pdf. Authorization [aw″ther-ĭ-za´shun] permission. insurance authorization in the nursing interventions classification, a nursing intervention defined as assisting the patient and provider to secure payment for health services or equipment from a third party. miller-keane encyclopedia and dictionary of medicine, nursing, and allied health, seventh. Dfec general medicalauthorization request (fax 1-800-215-4901) please read the instructions carefully bef ore completing medical authorization codes authorization request. complete all applicable fields. all prior code and procedure code is required for the outpatient revenue code, type or print applicable. (f) unusual travel expenses require prior authorization by the payer. the payer and billing provider shall agree upon maximum fees (cpt® code 99082). (g) medical testimony is covered under rule 18-6(d) and special reports are covered under rule 18-6(g)(3)&(4) (cpt® codes 99075 and 99080). parents often bring in forms for the physician to fill.
Define authorization. authorization synonyms, authorization pronunciation, authorization translation, english dictionary definition of authorization. Medicalauthorization and bill processing information on the process for submitting medical authorization medical authorization codes requests and bill. physician dispensed medication using unspecified "j codes" payment for medications billed under j3490, j3590, j7999, j8499,. Prior authorization for llps will be implemented in two phases. phase one will begin may 11, 2020 in one state from each dme mac jurisdiction: california, michigan, pennsylvania, and texas. phase two will begin october 8, 2020 and expands prior authorization of these codes to all of the remaining states and territories.
Medical prior authorization. prior authorizations: upmc health plan will be implementing an expanded approach to prior authorizations in collaboration with healthhelp for advanced radiology/imaging, cardiology, sleep, and musculoskeletal services. healthhelp procedure codes procedure code bundles policies and procedures. Vaccine code vaccine administration code(s) administration codes track which dose in the regimen is being administered. manufacturer vaccine name(s) ndc 10/ndc11 the national drug code (ndc) uniquely identifies human drugs in the united states; it can be found on the vial containing the vaccine. the 11-digit number may be required on claims submitted to third party payers. Welcome to the medi-cal provider home. under the guidance of the california department of health care services, the medi-cal fee-for-service program aims to provide health care services to about 13 million medi-cal beneficiaries.
Medical authorizations & claims authorization process. all requests for ccs diagnostic and treatment services must be submitted using a service authorization request (sar) form except orthodontic and dental services (all necessary authorizations will be medi-cal dental ’s responsibility). services ndc billing for hcpcs medical professional services medical authorization unit (mau) long-term care and waiver services hospitals health management program global messages molecular pathology fqhc pps rates fqhc-rural health clinics forms error codes/edit disposition codes ehr incentive provider enrollment electronic Physician dispensed medication using unspecified "j codes" payment for medications billed under j3490, j3590, j7999, j8499, j8999 and j9999 require prior authorization by claims staff. the strict exception based policy is described in circular 18-06. bills for these codes received on and after june 1, 2018 without prior authorization will deny. The updated list of codes that require prior authorization as a condition of payment can be found below. update 05/19/2020: cms will host a special open door forum call to discuss the prior authorization process and requirements for certain outpatient hospital department services on thursday, may 28, from 1:30p. m. to 3:00p. m.
Referral & authorization guidelines. medical prior authorization code list may 1, 2021 open a pdf; medical prior authorization code listfebruary 23, 2021 open a pdf; medical prior authorization code listfebruary 1, 2021 open a pdf; medical prior authorization code listjanuary 1, 2021 open a pdf; medical prior authorization code listnovember 1, 2020 open a pdf. Pre-authorization codes a complete list of the treatments and procedures that require providers to obtain preauthorization is available by clicking on the links below. this new list is in effect march 22, 2021. The term authorization is also referred to as pre-authorization or prior-authorization. it is a legal obligation to ensure that the insurance payer pays for the specific medical service mentioned in the medical claim form. As a medical billing professional, dealing with prior authorization is a necessary part of the job. prior medical authorization codes authorization (also known as preauthorization) is the process of getting an agreement from the payer to cover specific services before the service is performed. normally, a payer that authorizes a service prior to an encounter assigns an authorization